Supplement Series: Vitamin D (Part 3 of 5)
Welcome back to our 5-part expert series on Vitamin D.
In our last post, we talked about the importance of vitamin D in combating one of the leading causes of death across the globe, namely cardiovascular disease.
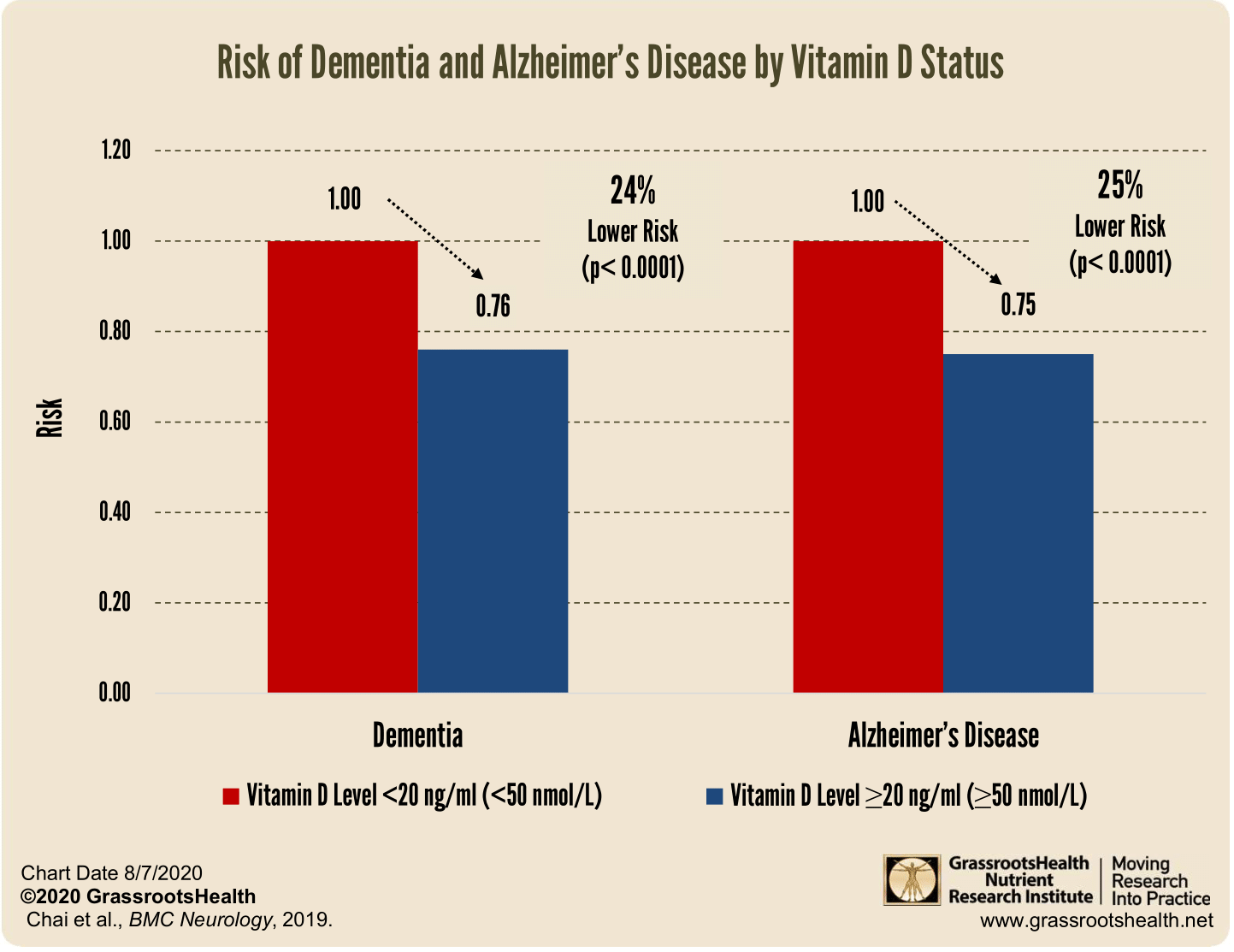
In part three of our vitamin D supplement series, we are focusing on the link between vitamin D and cognitive health. Studies have linked low levels of vitamin D to a higher risk of developing various mental health conditions, including Alzheimer's disease, dementia, schizophrenia and even those ‘senior moments’.
Let’s dive into the connection between vitamin D and cognitive health.
The Link Between Vitamin D and Cognitive Health
Vitamin D is essential for healthy brain function and development. It helps protect neurons from oxidative damage which can cause memory loss and other cognitive problems over time.[1,2] These neuroprotective benefits are also seen in both developing and adult neural tissue.[3,4] Low levels of vitamin D can impair neural plasticity, which is the ability for new connections to be formed within the brain. This is especially important for older adults as their brains become more vulnerable to neurological changes due to age-related decline. Studies have even shown that infants experiencing a lack of vitamin D in the womb suffer from long-lasting structural changes in the architecture of the brain.[5]
Low levels of vitamin D may also be associated with decreased grey matter volume in certain areas of the brain typically responsible for memory processing, learning and concentration.[6]
Vitamin D also plays an important role in protecting against inflammation throughout the body, including within the brain.[7] Chronic inflammation can lead to damage in brain tissue which can contribute to cognitive decline over time. A 2020 study found that low levels of vitamin D were associated with greater markers of inflammation in elderly individuals suffering from mild cognitive impairment (MCI).[8] MCI is defined as a state between normal aging processes and early stages of dementia or Alzheimer’s disease. The findings suggest that increasing levels of vitamin D may help reduce inflammation-related damage within the brain that could otherwise lead to further cognitive impairment down the line.[9]
What about psychiatric conditions?
Schizophrenia. This chronic disorder is characterized by hallucinations (auditory, visual), delusions and changes to cognition that impact daily living. In a small study published in 2021, 40 patients were given 50,000 IU weekly for 8 weeks and every measure of the condition improved when vitamin D levels were normalized.[10]
Mild Cognitive Impairment. This condition is often considered a precursor to later decline including areas of memory and executive function. One of the more layman terms for its symptoms is known as having a ‘senior moment.’ In a study of 80 elderly individuals, those with the lowest levels of vitamin D (4-16 ng/mL or 10-40 nmol/L) were 25x more likely to experience senior moments than those with levels of 32-76 ng/mL (80-190 nmol/L).[11]
Bipolar Disorder. The research on the link with bipolar symptoms ranging from manic to depressive is still developing, but early studies show promise. Youths diagnosed with BP were directed to take 2,000 IU daily for 8 weeks and researchers tracked a number of biomarkers including GABA and glutamate in the anterior cingulate cortex. There were improvements in these markers and significant decreases in Children’s Depression Rating Scale scores and Youth Mania Rating Scale scores.[12]
Brain-Derived Neurotrophic Factor
Vitamin D is involved in the production of brain-derived neurotrophic factor (BDNF), which plays an important role in overall neuron growth and much more. Low levels of BDNF have been linked to Alzheimer’s disease, dementia, schizophrenia, senior moments, memory loss and decreased brain matter volume. Conversely, higher levels of BDNF have been associated with improved cognitive function and memory performance. One study showed that having BDNF levels that were one standard deviation higher, one could reduce their risk for dementia and Alzheimer’s disease by 33%.[13]
How Can You Increase Your Vitamin D Intake?
As we discussed previously in this series, sun exposure is one way you can get an adequate amount of vitamin D naturally. However, depending on where you live or how often you are able to get out into the sun, it may not always be possible to get enough natural sunlight exposure for optimal levels of vitamin D production within your body. Therefore, it may be beneficial for some individuals to consider taking a daily supplement or eating foods that contain higher concentrations of this essential nutrient (e.g., fatty fish like salmon or mackerel). A registered naturopathic doctor or healthcare provider can provide additional guidance about how much and what type(s) of vitamin supplements will best suit your individual needs given your lifestyle factors such as skin tone/coloration and location/climate/time zone where you reside most frequently throughout any given year(s).
There is increasing evidence suggesting that there may be a correlation between low levels of vitamin d intake and negative effects on overall cognitive health – specifically related to memory formation/retention as well as long-term neurodegenerative disorders such as Alzheimer's Disease & other forms of dementia. Increasing your intake through dietary sources or supplementation (under the guidance & supervision of a healthcare professional) may help improve overall mental functioning & reduce risk factors associated with developing these complex diseases down the line – making now a great time to start exploring ways to boost your own level!
We hope you learned something new today! Join us next time for a conversation on vitamin D status and metabolic function.
References
Chopp, Michael, Zheng Gang Zhang, and Quan Jiang. "Neurogenesis, angiogenesis, and MRI indices of functional recovery from stroke." Stroke 38.2 (2007): 827-831.
Brewer, Lawrence D., et al. "Vitamin D hormone confers neuroprotection in parallel with downregulation of L-type calcium channel expression in hippocampal neurons." Journal of Neuroscience 21.1 (2001): 98-108.
Tetich, M., et al. "Neuroprotective effects of (24R)-1, 24-dihydroxycholecalciferol in human neuroblastoma SH-SY5Y cell line." The Journal of steroid biochemistry and molecular biology 89 (2004): 365-370.
Stewart, Adam, et al. "Neurosteroid vitamin D system as a nontraditional drug target in neuropsychopharmacology." Behavioural pharmacology 21.5-6 (2010): 420-426.
Eyles, Darryl, et al. "Vitamin D3 and brain development." Neuroscience 118.3 (2003): 641-653.
Beydoun, May A., et al. "Vitamin D, Folate, and Cobalamin Serum Concentrations Are Related to Brain Volume and White Matter Integrity in Urban Adults." Frontiers in aging neuroscience 12 (2020): 140.
Magrone, T., G. Marzulli, and E. Jirillo. "Immunopathogenesis of neurodegenerative diseases: current therapeutic models of neuroprotection with special reference to natural products." Current pharmaceutical design 18.1 (2012): 34-42.
Lee, Do Hun, et al. "Association between vitamin D deficiency and cognitive function in the elderly Korean population: A Korean frailty and aging cohort study." Medicine 99.8 (2020).
Moon, J. H., et al. "Serum 25‐hydroxyvitamin D level and the risk of mild cognitive impairment and dementia: the Korean Longitudinal Study on Health and Aging (KL o SHA)." Clinical Endocrinology 83.1 (2015): 36-42.
Neriman, Aras, Yilmaz Hakan, and Ucuncu Ozge. "The psychotropic effect of vitamin D supplementation on schizophrenia symptoms." BMC psychiatry 21.1 (2021): 1-10.
Annweiler, Cédric, et al. "Vitamin D insufficiency and mild cognitive impairment: cross‐sectional association." European Journal of Neurology 19.7 (2012): 1023-1029.
Sikoglu, Elif M., et al. "Vitamin D3 supplemental treatment for mania in youth with bipolar spectrum disorders." Journal of child and adolescent psychopharmacology 25.5 (2015): 415-424.
Ng, Ted Kheng Siang, et al. "Decreased serum brain-derived neurotrophic factor (BDNF) levels in patients with Alzheimer’s disease (AD): a systematic review and meta-analysis." International journal of molecular sciences 20.2 (2019): 257.